Bunion Deformity
Bunion Deformity (Hallux Valgus)
 While mostly hereditary, bunions are also the unattractive and often painful end-result of fashionable footwear and a history of shoe choices that have habitually fit the fancy of the wearer more so than the foot.
While mostly hereditary, bunions are also the unattractive and often painful end-result of fashionable footwear and a history of shoe choices that have habitually fit the fancy of the wearer more so than the foot.
While some are willing to make such a sacrifice for a designer name far more difficult to pronounce than the affliction they can cause, many simply do not realize that shoe choice can be such a significant contributor to bunion deformity and pain. But it is, in fact, all about shoe choice in both those genetically predisposed and those who are not – as rarely have bunions been identified in those who do not wear shoes.
What is a bunion?
 Bunions are a common foot condition that affect many in today’s busy society. While much more common in women than men, they are equally painful and potentially debilitating. Some bunions may not hinder daily activity greatly, while others can dramatically impact foot function.
Bunions are a common foot condition that affect many in today’s busy society. While much more common in women than men, they are equally painful and potentially debilitating. Some bunions may not hinder daily activity greatly, while others can dramatically impact foot function.
Although commonly painful on its own, a bunion is actually a consequence of the outward deviation of the big toe, which doctors call Hallux Valgus or HV.
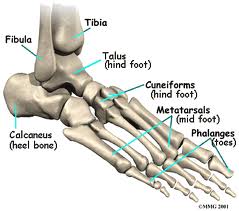
Hallux is the medical term for the big toe, and valgus the outward direction it turns as the deformity develops. As the big toe moves towards the small toe (into valgus), a bump appears over the inner edge of the metatarsal bone, which is no longer in line with the big toe. This is what is commonly called the bunion. Left untreated, it generally worsens and can greatly hinder day to day life and the ability to fit into any shoe.
What causes HV?
Bunions are commonly hereditary, the result of several anatomic abnormalities such as instability of the first tarsometatarsal joint, an idiopathic gastrocnemius contracture (IGC) or Achilles tendon contracture, pes planus, also known as flat foot, and an excessive separation or angulation between the shafts of the first and second metatarsals, referred to as the intermetatarsal angle. The intermetatarsal angle can be thought of as a forefoot in which the metatarsal (foot bone) alignment resembles the metacarpal alignment of the hand. The presence of these abnormalities can be further agitated by the wrong footwear selection – and usually result in the most severe deformities.
 Less severe cases of HV are more commonly seen solely as the result of shoe wear – size and shape – and its effect on the foot. Fashionable women’s shoes commonly tight and pointy will push the hallux into valgus. High heeled shoes most women (and men) find attractive will create or exacerbate an idiopathic gastrocnemius contracture (IGC) and worsen. HV rarely occurs in individuals who do not wear shoes.
Less severe cases of HV are more commonly seen solely as the result of shoe wear – size and shape – and its effect on the foot. Fashionable women’s shoes commonly tight and pointy will push the hallux into valgus. High heeled shoes most women (and men) find attractive will create or exacerbate an idiopathic gastrocnemius contracture (IGC) and worsen. HV rarely occurs in individuals who do not wear shoes.
How is HV treated?
The treatment for bunions depends on the severity and amount of pain, discomfort and disruption to daily activity. Some cases are addressed simply by changing the size and shape of the shoes regularly worn. We recommend that women wear flat, roomy shoes as much as possible – carrying pumps along to change into when the occasion demands. Stretching the gastrocnemius and heel cord is always necessary. Commonly shoes with arch supports or an orthotic can help in people with abnormalities such as flat feet or low arches.
When these measures are not successful, surgical treatment may be necessary. The key to successful surgical treatment and the best possible outcome is accurate identification and measurement of all anatomic abnormalities. If this does not occur, HV will invariably recur.
The type of HV surgical repair best for each patient depends on the cause. The issues considered in making the decision include:
- The severity of the bunion deformity
- Presence of an angular deformity of the first big toe bone (metatarsal or the proximal phalanx)
- Presence of arthritis in the first big toe (metatarsophalangeal) joint
- Presence of associated deformities in the lesser toes, such as hammer toes, cross-over toes or pain under the lesser metatarsal heads
- The size of the intermetatarsal angle
- The stability of the first tarsometatarsal joint
- The presence of a flat foot
- The presence or absence of an idiopathic gastrocnemius (IGC) or Achilles tendon contracture
Feet severely arched and strained in high heeled shoes.


Feet at ease in ballet flats.


What are the different surgical procedures used to correct Hallux Valgus?
The different types of surgical repair of HV depends on the anatomic abnormalities and severity and may include:
Soft tissue surgery
Distal soft tissue procedures, also commonly known as the Silver procedure includes, an exostectomy and an incision in the space between the first and second metatarsals to release the adductor tendon and the capsule of the metatarsophalangeal joint. As an isolated procedure it is found to be limited, though effective when used in conjunction with osteotomy and fusions when the Hallux Valgus cannot be passively corrected by manually positioning the big toe in the normal position.
The Strayer procedure is performed by releasing the tendon of the gastrocnemius just above where it merges with the soleus tendon to form the Achilles tendon. While by itself it will not correct the HV deformity, it will help prevent its recurrence and the development of other painful conditions in the foot.
Osteotomy
Among the different types of procedures used to correct HV deformities, nearly all will include an exostectomy, which is the shaving down of the bump on the inside of the first metatarsal – commonly referred to as the bunion. Simple removal of the bump is rarely successful except in the very elderly. Most commonly, it is performed in conjunction with a cut of the first metatarsal bone, which is called an osteotomy.
For milder bunion deformities with no other severe anatomic abnormalities, distal metatarsal osteotomies are performed, which is an osteotomy done at the end of the metatarsal. More severe bunion deformities may require a proximal osteotomy, which is an osteotomy done at the base of the first metatarsal or an Arthrodesis (fusion) of the first tarsometatarsal joint also known as the Lapidus procedure. Dr. Sanders commonly uses the Ludloff osteotomy when a proximal osteotomy of the metatarsal is needed.
The chevron osteotomy is one of the more common distal metatarsal osteotomies performed and involves a V-shaped bone cut made in the metatarsal – allowing the bone to be shifted over. The remaining edge of the bone is shaved down. A small screw or pin is inserted into the bone to hold the metatarsal head in place and accelerate bone healing. Walking is generally permitted (using a surgical shoe) the day following a chevron osteotomy – and is worn for six weeks before patients are allowed to wear comfortable walking shoes.
Occasionally, there is also a deformity of the proximal phalanx (first big toe bone). In these cases, the metatarsal osteotomy procedures can be “supercharged” by performing an osteotomy of the proximal phalanx. This procedure is known as the Aiken procedure, and can add an additional 10 degrees of correction. It too, is stabilized with a screw or a pin. When this is preformed, both osteotomies will heal at the same time without increasing the post-operative pain or restrictions.
Proximal metatarsal osteotomies are used to correct more advanced HV deformities when the intermetatarsal angle is excessive. In these cases the angular deformity is corrected closer to is apex. The exact type of osteotomy required depends on the amount of deformity. The bone is stabilized by the insertion of several screws. A distal soft tissue procedure is commonly performed in conjunction with a proximal osteotomy. Occasionally an Aiken osteotomy is also performed. Walking is generally permitted (using a surgical shoe) the following day – and is worn for six weeks before patients are allowed to wear comfortable walking shoes.
Arthroplasty
When patients have arthritis of the big toe joint, which is associated with a bunion deformity, an arthroplasty is performed rather than an osteotomy. An arthroplasty removes a portion of the proximal phalanx. It is most useful in elderly patients who do not spend much time on their feet. Arthroplasty with implants have been attempted for decades. To date, none have passed the test of time and we highly recommend against them.
Fusion
Severe HV deformities with instability of the first tarsometatarsal joint and considerable angulation between the first and second metatarsals require correction. This procedure is indicated in cases in which deformities in the lesser toes, such as hammer toes, cross-over toes or pain or callosities under the lesser metatarsal heads is present. In these cases, the first tarsometatarsal joint in between the first metatarsal and the cuneiform bone is fused with screws, which realigns the metatarsal completely and stabilizes the bone and recurrent deformity. This is known as the Lapidus procedure.
Fusion of the big toe joint is also an excellent option for patients with severe bunion deformity and arthritis of the joint, as it reliably relieves pain, corrects the deformity and prevents the bunion from returning. The one disadvantage of this procedure is that it limits shoe wear to flat shoes, making it more advantageous for males.
When considering surgical correction of HV, the most important aspect is a thorough assessment and selection of the best procedure for your particular case. A “one size fits all” surgical approach is destined to failure, because every HV deformity is a bit different. Unfortunately, what many doctors have learned in their training has proved limiting.
It is important to choose a foot and ankle surgeon who is fully trained in making the right anatomic diagnosis and able to institute the appropriate corrective measures. Frequently, this will involve repair or reconstruction of structures beyond the bunion and the laterally deviated big toe. Dr. Sanders has no “preferred” procedure he performs in the treatment of bunions, something that is, unfortunately, common among many Orthopedists and Podiatrists alike. In keeping with his overall approach to treating patients, he customizes the procedure to the patient.
